Archive for category Children
How safe vaccines led to the resurgence of pertussis
Posted by Nick Bennett MD in Antivax, Children, Public Health, Vaccines on August 21, 2012
For those who haven’t been under a rock recently, several parts of the US have seen a surge in pertussis cases. Much of this has been (fairly) blamed on anti-vaccination efforts to reduce herd immunity and the cocooning of vulnerable infants. But that’s not the whole story.
Interestingly enough, it’s now clear that the DTaP vaccine (diphtheria, tetanus, acellular pertussis) doesn’t provide long-lasting immunity. We had some clues with this as an awareness grew of pertussis in older teens and adults, fueled in part by vastly improved testing for pertussis (PCR versus ‘cough plates’ for culture) and a recognition that pertussis in older kids and adults didn’t look like the classic ‘whopping cough’ that youngsters got.
A booster dose of pertussis vaccine was recommended, included as part of the tetanus booster (the new Tdap vaccines). Recent outbreaks seemed to focus on the group of kids aged 10-11 years of age – when vaccine immunity was waning, but just before their Tdap booster – but the recent outbreak in Washington State has involved even 13-14 year olds, who did get their booster!
The question then should be – why does the NEW vaccine work LESS well? The answer is because it is SAFER.
The old DTP vaccine began to get a bad reputation for neurologic disease – in fact a contraindication still exists to withhold pertussis-containing vaccines in kids who develop neurologic issues after pertussis vaccination, even though the vaccine is different. The old DTP contain literally thousands of antigens, based as it was on a relatively impure cocktail of cell culture fragments that contained the pertussis bacteria. It caused a fair amount of immune reaction, and clearly was linked to febrile seizures.
Several high-profile cases of apparently neurologically damaged children (leading to the formation of some of the early modern anti-vaccine movement) pushed the vaccine manufacturers to create a cleaner vaccine, an ‘acellular’ pertussis vaccine, which is why we have DTP and DTaP. DTaP doesn’t have the same link of febrile seizures and no link to any neurologic issues (interestingly, as detailed in Paul Offit’s book on the history of antivaccine junk science, neither do any of the original DTP kids…it was all a big screwup). Tdap is even less immunogenic as it has slower concentration of antigens – you can tell this because it has a small “p” instead of a big “P”. True story.
The trouble of course is that by having a less inflammatory response, with far fewer antigens, the protection is less. The original DTP vaccine contained more antigens than the ENTIRE modern vaccine schedule does, several times over. Any statement about ‘too many too soon’ is pure bunk – our kids are exposed to fewer vaccine antigens in their entire schedule that we were in one vaccine.
This story highlights several points – firstly, contrary to antivax propaganda, not only are there mechanisms in place to detect and respond to potential vaccine side effects but there are CHANGES made to the vaccines in an attempt to keep people safe. (Probably the only positive thing to come out of the antivax movement is the establishment of the Vaccine Adverse Event Reporting System, VAERS). Secondly, there are compromises to be made – more effective sometimes also means more side effects, so if you want to lower one you may end up lowering the other.
There is also data from Europe that as the vaccine strains of pertussis wane, there is strain replacement with potentially more virulent strains. So although we are seeing fewer cases, those cases we do see may be more serious (this finding hasn’t yet held true for the US…as far as I know).
Of course the antivax brigade have twisted the story yet again “Whooping Cough Epidemic Caused by Virulent New Pertussis Strain—And It’s the Result of Vaccine” shouted one headline. While technically true it doesn’t really go into the real explanation of WHY…even more impressive, but entirely unsurprisingly to me, the actual article the antivax site uses to support their claim starts with the words “Before childhood vaccination was introduced in the 1940s, pertussis was a major cause of infant death world- wide. Widespread vaccination of children succeeded in reducing illness and death.” which not only proves how disingenuous antivax proponents are, but how stupid they are. The first rule of selective quotation is to use sources that support your argument.
Sadly, those who believe antivax propaganda are not usually stupid – if anything they tend to be more educated than average, and well read. They just read the wrong things. Not everyone can go to medical school after all.
Then again, even that isn’t foolproof. One of the original antivax “Expert” witnesses from the UK trials that showed the DTP link with neurologic illness to be wrong went on to further his infamy with AIDS denialism.
Much of the details on the stories of the DTP and DTaP history are in Paul Offit’s book – Deadly Choices, which I highly recommend. In it he not only details how antivax proponents twist science and the facts to suit their case, but also how they nearly brought down the entire US vaccine industry through irresponsible and indefensible litigation. The vaccine WORKS to reduce serious illness from pertussis and undoubtedly saves lives. It’s not perfect, no one has ever said a vaccine was perfect – at least, not unless they were trying to make a point that it wasn’t…
Counterintuition – why neonatal herpes turns logic on its head
Posted by Nick Bennett MD in Children, Guidelines, Infections on August 9, 2012
“No maternal history of herpes”
When dealing with a newborn baby with a fever, those are words that strike fear into my heart.
Wait, what? You said no maternal history? Yep, that’s right.
Neonatal herpes simplex virus (HSV) is a topic that is full of counterintuitive statements, and far too much confusion. The wrong people get tested, the wrong people get treated, the wrong babies get worked up aggressively. When other docs diligently rattle off the “pertinent” aspects of the maternal history and clinical examination of the baby, in my mind I’m mostly saying “Don’t care, don’t care, don’t care….” before I interject and ask about test results that often haven’t been ordered.
Based purely on a numbers game, thanks to things like vaccination and Group B Strep prophylaxis, many early onset infections in newborns have been reduced. There is simply less infectious disease hanging around. But as a result, viral infections like neonatal herpes are proportionately becoming larger players – in some hospitals it is as common as bacterial meningitis. And neonatal HSV is a killer.
HSV comes in three distinct flavors – the least lethal is skin-eye-mucus membrane (SEM) disease. This is how many people expect to see herpes – a rash, typically vesicular (clear fluid-filled little blebs) and maybe some eye discharge or mouth sores. Most pediatricians, if they see something like this, appropriately freak out a little bit. SEM disease by itself isn’t too dangerous, and if treated properly is almost never fatal. Herpes is tricky though – in babies it can mimic other rashes, so you really do need a low threshold to consider it. ANY neonatal rash that doesn’t fit a normal neonatal rash (so know your neonatal rashes!) deserves a workup. There is nothing more sobering than to run a case of a neonatal rash by an ID doc and to have them tell you with complete sincerity that “You can save this baby’s life. Get them to an ER. Now.” Untreated SEM disease can progress to infection of the brain.
The most obvious presentation is disseminated disease – which weirdly enough can occur before SEM disease…first week of life or so. The kids are sick – really sick. They can be in shock, bleeding, in liver failure and struggling to breath as the virus overwhelms pretty much every organ system. The problem here is that even faced with this situation bacterial infection is considered immediately, and herpes can still be overlooked or thrown into the mix as an afterthought. Again, good neonatologists and pediatricians will be all over this from the start, having experienced their share of disasters in the past. Disseminated herpes is mostly fatal without treatment – and even with therapy about a third will still die, many of the survivors left with significant disabilities.
The last type of herpes infection is of the brain. Typically presenting later in the neonatal period (3-4 weeks of age, rarely later) herpes encephalitis of the newborn is devastating. Herpes causes a hemorrhagic encephalitis, meaning that it chews your neurons up into a bloody pulp. To a brain that has barely begun its developmental process, this is a disaster. Even if the baby survives they may be blind, deaf, paralyzed or have significant developmental delays.
From how I describe it above you might assume it would be easy to spot these kids. Well, it is – once it’s too late. The success of treating HSV depends to a large extent on how quickly you can start acyclovir – one of the few medicines we have that can treat viral infections (it’s pretty much only used for HSV). Acyclovir can shut down virus replication, but does nothing for those cells already infected. The difficulty with HSV lies in the nuances of the medical history.
Let’s try some armchair science for a bit. Would you, as a baby, rather get HSV from a mother who is having a recurrent outbreak of HSV, with low-levels of virus, and have her give you antibody protection through the placenta…or would you prefer to catch HSV from a mother who is having her FIRST outbreak (which may be without symptoms) with high-levels of virus and no antibody protection? Well, you may ask, how likely is that? The answer is Very. About 90% of all neonatal HSV cases come from mothers with no history of HSV. If your mom DOES have HSV and has a recurrent outbreak, the risk of transmission is about 5%. For a new case – its closer to 50%. Maternal history of HSV is relatively PROTECTIVE for the baby.
But the focus is on the mothers who test positive for HSV during pregnancy. They get put on valtrex (an oral version of acyclovir which is well absorbed), when it has not been shown to sufficiently reduce transmission. They may get a C-section, when that hasn’t been shown to help either (except maybe in the case of active lesions at the time of delivery…and even then it’s unreliable). The mothers who are HSV-negative are ignored, when they are those at highest risk of passing HSV to their babies. In an ideal world, their sexual partners should be tested and if THEY are positive THEY should be put on valtrex to reduce outbreaks and educated about the risks. But the fathers aren’t the patient….so nobody does that.
A big myth about HSV is that all babies with it look sick. Well, they do eventually – but to start with they look pretty normal. I have heard docs say that a baby looked “too good to tap” – meaning they didn’t perform a spinal tap to check for meningitis or HSV encephalitis. Or they don’t test sufficiently for HSV, or don’t start treatment with acyclovir while test results come back (these same babies are almost universally started on antibiotics for presumed bacterial infection). Published case series of proven HSV cases shown over and over again that babies with HSV present with relatively innocuous symptoms. “poor feeding” “fever” “sleepiness” before the more obvious symptoms of “shock” “seizure” or “respiratory distress”. Remember, by the time the baby is sick from HSV the damage has already been done, and you can only try to stop it from getting worse and hope the kid recovers. With bacterial infections we can kill them directly with antibiotics and the damage is usually secondary to the infection, and not because the bacteria are literally eating up your cells and blowing them apart as HSV does. Even with successful treatment, symptomatic HSV in babies has a slow recovery.
So how do you deal with this uncertainty? You can’t trust the mothers history, you can’t trust the baby’s physical examination or symptoms…what do you do?
My approach is to have a low threshold for suspecting HSV in neonates. ANY baby getting worked up for a possible bacterial infection needs to have a workup and empiric treatment for HSV as well. Babies with weird symptoms (especially rashes or neurologic symptoms) need to have HSV considered FIRST, before bacterial causes. HSV is not only potentially devastating – its treatable, and therefore the bad outcomes are preventable.
Fortunately the Committee of Infectious Diseases of the American Academy of Pediatrics has published recommendations – albeit in a rather inaccessible set of paragraphs. I can summarize them here though:
Spinal tap for HSV PCR of spinal fluid.
Liver enzyme testing for disseminated disease – chest x ray if respiratory symptoms.
Surface cultures from eye, mouth, rectum and any skin lesions.Start acyclovir – do not stop until all tests are negative.
Do ALL of this this for EVERY BABY with suspected HSV.
Repeat spinal tap on kids with positive CSF to ensure clearance after 21 days – continue therapy if still positive.
A big mistake I see people making is in testing the spinal fluid to “rule out HSV” but do not doing the rest of the workup. Spinal fluid testing for HSV no more rules out SEM or disseminated disease than a urine culture can diagnose meningitis. I have seen cases missed (or nearly missed) because someone didn’t do the whole thing. You NEED the liver enzyme testing to rule out disseminated disease, and it matters. Treatment for simple SEM is 14 days – treatment for disseminated or CSF disease is 21 days. I have seen a handful of kids with positive CSF tests but with totally normal looking spinal fluid (eg no white cells, normal protein levels etc).
The trouble is HSV, as bad as it is, isn’t all that common among the hundreds of kids you will see with suspected neonatal infection. And many of THEM will be obviously HSV. So many kids get a semi-workup and we get away with it because “whoops, the CSF is positive!” and you treat for 21 days even though you didn’t check the liver enzymes.
But I’ve also seen the opposite – kids who were partially worked up and the diagnosis was missed, or delayed, or the severity was under-appreciated. All too often the “standard of care” let’s these kids slip through the cracks – which is inexcusable in my mind when there are experts who put it down in writing exactly how to work up these cases.
So let’s raise the standard.
Totally useless history:
Mom has no history of HSV
Mom got Valtrex
Mom got a C-section
Baby looks well
REAL risk factors for neonatal HSV:
Prolonged rupture of membranes
Active lesions at time of delivery
NO maternal history of HSV
Prematurity
Age less than 21 days
Unusual rash
Seizures or lethargy
“Sepsis” not responding to antibiotics (oops! too late! – better call your lawyer…)
Testing
CSF PCR
PCR/Culture of skin lesions, eyes, mouth, rectum
Liver enzyme testing
Chest X ray (if symptomatic)
Treatment
Acyclovir 20mg/kg/dose IV every 8 hours
Until all tests are negative (typically 2-3 days empirically)
14 days for proven SEM disease
21 days for disseminated or CNS disease
And if you’re not sure…get a consult…
Nearly done
Posted by Nick Bennett MD in Career, Children, Medical Education on September 5, 2011
I’m awake.
It’s early.
I don’t have to be awake, but I can’t sleep. You see, this is my last day of service.
Not my last day of work – no, I have that tomorrow – but for whatever reason my mind is aglow with whirling transient nodes of thought (Blazing Saddles reference for you) and I can’t get back to sleep. I’ve just caught up with some outstanding dictations (outstanding in that they are late, not that they are in any way good) and so I thought I’d reflect a bit.
I’ve been at Upstate for the past 7 1/2 years. I showed up here as a medical student, post-PhD, not yet done with my medical training and not yet certain about even doing Pediatrics as a career. I had set up a month-long elective in Pediatric Infectious Disease because (A) my one and only US medical contact was a Peds ID faculty member and, er, that was it. I figured I should brown-nose a bit.
No seriously, that was it.
At the end of that month I had somehow got the next 7 years all planned out… This guy hired me to work for him doing research and clinical trials for a year. I took my USMLE exams. I applied for residency (Upstate was the only place I applied to). It was taken for granted that I would transition into the ID Fellowship, which I did, so I have just been part of the furniture here for all that time.
I have seen the new Children’s Hospital grow from a mythical idea to scaffolding to wonderful newly equipped spacious rooms. I have supervised medical students, watched them grow as Residents and young people, and seen them graduate and start work as Faculty. I have made mistakes, learned a lot, learned that I have a lot still to learn, and I like to think that somewhere along the way I saved a few lives. I’m not sure I’ve actually achieved anything quite so grand – but I’m pretty sure I had a positive impact on an awful lot of kids.
I certainly can’t claim to be the world’s best resident – I have had plenty of peers and colleagues who were better doctors than me: more knowledgeable, more intuitive, harder working, better at getting IV’s started…but I have found that I am good at what I do. I am good with patients and families, I actively practice patient-centered care, I can teach effectively and I can do research. Give me a database and a few hours to code and I can churn out some cool stuff.
It’s a weird feeling to move on – to a job where there are things to get done, where I won’t have the kind of supervisory backup that I’ve enjoyed as a trainee, but where I’ll also have the freedom to practice medicine and work more along my own path. The light at the end of the tunnel has turned out to be an oncoming express train…and I don’t think it truly hit me (pardon the expression) until the past few days. My last 2 weeks of service have been too busy to think about it! Now suddenly, here I am, wrapping up my last dictations and preparing my last lecture. I need to bring boxes to my office to empty it: how weird is that? There are an awful lot of really, really cool people I’m going to miss at Upstate. Nurses, lab techs, pharmacists, Docs – so many people who I’ve worked with over the past few years and got to know. They shaped how I practice medicine. I think that may be the most intimidating thing about having to move – having to re-learn all the ways and intricacies of a new system, a new place. I’ll be flying blind for a bit. I figure it’s worth it.
The thing to remember, and this is a crucial thing for any aspiring doctors to realize, is that I really enjoy what I do. Whatever fluke of fate brought me to Upstate and Peds ID, I can truly say that I don’t think I’d be happier doing something else. Pediatrics wins over any adult care for me, every time. And Infectious Disease…? There’s just something about finding a cause for a disease and killing it. You can’t do that for hypertension, or asthma, or obesity, or diabetes – “You’ve got the bugs, we’ve got the drugs” became my catchphrase.
Confucius said “If you love your job, you’ll never work a day in your life.” He was right.
Gardasil hysteria plays into hands of pediatricians
Posted by Nick Bennett MD in Antivax, Children, Public Health, Vaccines on August 13, 2011
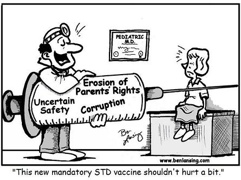 Cartoon by Ben Lansing – from Age of Autism website
Cartoon by Ben Lansing – from Age of Autism website
Stories like this one at anti vaccine sites are unfortunately typical in their misinformation and use of hyperbole and sound bites rather than informing the reader in a non-biased manner. What I found amusing is that the specific approach used in this article actually plays into the hands of pediatricians…
Let’s ignore the rhetoric of the “dangerous” HPV vaccine (it is not) or the claim that it has caused “as many as twelve deaths in the US alone” (it has not) and focus on the headline of the piece.
“California mulls giving 12-year-olds STD vaccine Gardasil without parental consent”
While being technically correct that Gardasil does indeed protect against a sexually transmitted virus, the implications here are clear – anything involving 12 years olds and STDs is immoral, and anything where the parents have no say is unethical. Putting the two together is an order of magnitude worse!
Far from implying that 12 year olds are “sexual animals” (their words, not mine) the simple fact is that the 11-12 year old well-child visit is a perfect time to address many aspects of preventative care before the child becomes a teenager. This is why the vaccine is recommended at 11 years even though it is approved down to 9 years of age. Updating the vaccines at that visit is a no-brainer. With any luck the kids are NOT YET “sexual animals”, because ideally you want to protect them before that happens. Getting the HPV shots started 6 months before a teen’s “big night” is, I’m sure, not something they have on the calendar…and having taken care of my share of teenage mothers I can vouch for the fact that planning their sexual activity is clearly not something they are very good at at all.
Sexual health for teens includes proper counseling, education, and access to contraception. Abstinence is the most obvious way to avoid STDs and unwanted pregnancies, but abstinence-only education is associated with HIGHER rates of pregnancy and SIMILAR rates of STDs than more well-rounded education! Over half of abstinence “pledgers” will still go on to have pre-marital sex, the same rate as teens who don’t pledge abstinence (80% in fact denied ever having pledged in the first place…) While there may be an initial delay in the first sexual episode, after that the lack of proper education really does these people a disservice (if they are delaying sex, but their STD rates are similar, then someone is playing catch-up!) Not giving them a vaccine that, if all three shots are given on time, protects against 70% of cervical cancer is simply wrong.
The second part is whether or not parents have a say. In general, parents operate under the assumption that they are responsible for the health and well-being of their child until they are an adult. They get to call the shots (pardon the pun) and have access to all the information. Sadly, as some discover, that simply isn’t true. Parents do have the responsibility to take care of their kids, but if they fail to do so then the authorities can step in and take over that responsibility – most obviously in cases of child abuse or neglect. Effectively the State acts as if it is responsible for the welfare of children and merely delegates that responsibility to the kids’ parents or legal guardians – a delegation they can revoke if need be. But a lesser known area where parents lose their right to control their kid’s healthcare is sexual health.
It is clear that in order for teens to feel safe about coming forward to ask for help with sexual health issues, this MUST be done under strict confidentiality. Having a requirement that parents provide consent to treat (as is needed for every other situation except life-threatening emergencies) is a barrier to effective safe treatment of teens sexual health issues. The laws vary by State but in many places minors are allowed access to confidential sexual healthcare.
Ironically perhaps, by trying to demonize Gardasil as a way in which the medical establishment is sexualizing the youth of today, and labeling it explicitly as a sexual health vaccine, antivax groups are automatically putting it outside the remit of parental oversight. In the same way as a sexually active teen can (and should) get advice, contraception or treatment for STDs without fear of their parents knowing about it, I see no reason why they shouldn’t be allowed to ask for a sexual health vaccine under the same existing laws.
LEAPP-ING to childrens’ defense
Posted by Nick Bennett MD in Children, Patient-Centered Care on August 10, 2011
Several years ago, before our children’s hospital was built, I remember spending time chatting with one of our child-life specialists about various incidents in the hospital. And by “chatting” I mean rants about procedures or events that involved some degree of non-patient-centered care.
This wasn’t just your every-day “I didn’t ask them what they thought of the plan” kind of failing, this was the “we do this procedure on adults all the time in the office, so we’re not going to use pain meds on your 3 year old” kind of failing.
There were various kinds of issues. The “treating kids like small adults” was just one, others included the “sneak attack” where doctors (usually surgeons) would rush into a patient’s room, and perform some kind of invasive procedure – whether it be a dressing change, a drain removal, or some other kind of “quick” thing – that would often degrade into a messy charade of “we’re nearly done” and “this doesn’t hurt” while the nurses are stat-paging child-life to come sort out the screaming child. Sometimes even a relatively well planned attempt would fall flat due to missing items or drugs wearing off. Some procedures, which I shan’t reveal here for risk of HIPAA violation and upsetting my readers too much, were nothing less than torture.
As it happens, she and I were far from the only ones thinking about this. One of the pediatric Attendings who was working on a project grant for child advocacy, one of my co-residents (now an Attending in her own right) who helped teach my Communication Skills course, and a couple of nurses were also keen to fix things. Several brain-storming sessions later we came up with the core idea, and our residency director (grabbing coffee outside the meeting room and overhearing us) coined the acronym – LEAPP.
Listen – Evaluate – Anticipate – Plan – Proceed.
Listen – to the concerns of the parents, the nurses, and the patient. Does this child have a specific fear or pattern of behavior, or coping strategy? What worked well, or didn’t, in the past?
Evaluate – the current situation. Has this child already gone through a traumatic event, such as a burn, amputation or other situation that puts them at high risk for Medical Traumatic Stress? What is their current pain level? How anxious are they?
Anticipate – what could go wrong? What if the child acts out? Should we have a plan B? What kinds of non-pharmacological and pharmacological interventions can we use to reduce pain and anxiety?
Plan – get your stuff together, get the treatment room ready (patient beds are NOT the place to do procedures – they should be the one safe haven a kid has in the hospital), get the people ready: doctors, nurses, child life. Who is going to be “the voice” for the child during the procedure? How long will this take? Have enough meds ready to hand without needing more from pharmacy.
Proceed – only when everyone, including the patient, is ready. This means waiting for meds to take effect!
This grand ideology, invented in a small conference room by half a dozen disparate people of entirely different roles, got itself some legs. We did research, surveys of the parents, doctors and staff as they performed procedures on the floor. We drew up plans to teach these principles, created quizzes and slides, and somehow convinced the Graduate Medical Education Office to put it online for us. We scripted, acted and filmed an educational video to illustrate the points, with interviews from the best patient-advocates we knew – the big-time surgical and ER pediatric faculty who could lead by example to teach their residents what was REALLY important in medicine: caring for patients.
At some point an email came my way with a hospital policy on it. And I blinked.
Hospital policy. An institutional policy for pediatric procedural pain management. And I looked at what we had done.
It had taken us two years, but we had created a mandatory educational initiative for EVERY resident (not just pediatric residents) at our hospital. We had made it hospital policy to LEAPP for every pediatric procedure – meaning that if a resident or attending didn’t follow it, they were in breach of an OFFICIAL policy. This wasn’t touchy-feely stuff any more – this was serious.
I was stunned. I had heard the phrase – “Never doubt that a small group of determined individuals can change the world – indeed, it is the only thing that ever has” – but until that moment I had never really seen it in action.
Now you can walk about our shiny, roomy, children’s hospital and see our green froggy sticker on patient rooms who are due to have a procedure. The LEAPP manual is at the nursing station. Child Life is no longer performing damage limitation, but instead is preventing the damage from occurring in the first places. Nurses and doctors are working together to best plan how things should be done.
At least, they should be. There have been hiccups. We’d like to think things are better.
But you know what….we’re doing a survey about that.


