Posts Tagged powassan
Powassan virus – an “uptick” in cases, or simply better awareness?
Posted by Nick Bennett MD in Nick Bennett MD, Public Health, Uncategorized, viruses on May 9, 2024
A recent headline caught my eye, discussing an increase in the annual reported cases of Powassan virus – a virus which (for reasons that will become obvious) is near and dear to me. I decided to take a look at the actual data in more detail, and discuss a bit of that here, because understanding viruses like Powassan has implications beyond just this one infection.
Let’s start with what Powassan virus really is – it’s an arbovirus, meaning transmitted by arthropods (in this case, Ixodes ticks), and has an ability to cause a form of encephalitis. It is in fact closely related to the Tick Borne Encephalitis (TBE) virus, but Powassan virus was actually named after the town in Ontario where it was first discovered. It’s highly likely that many (perhaps the majority) of infections don’t go on to cause very serious disease, but the actual risk of encephalitis from it is unknown because the total number of cases isn’t really known. Of the symptomatic cases, about half are quite serious and 10% are fatal. The CDC has made it a nationally reportable infection, but the tricky part is knowing when to even think about it…
I diagnosed the first ever case of Powassan in Connecticut in 2016. It really was a bit of a crazy story, and truly a perfect storm of being in the right place at the right time. A young infant boy was admitted to the ICU with seizures and a very clear story of a few hours of a tick being attached to his leg 2 weeks earlier. The tick was brought into the house on a family member’s clothing, and probably got onto the child during a feed while being held by this person. The medical team had quite correctly ruled out most tick-borne infections due to the very short attachment time, but I knew that there was one exception – at least in animal models, Powassan virus could be transmitted in as few as 15 minutes. So it was possible, but was it probable? The clincher was the MRI report, which had a very distinct pattern showing “restricted diffusion of the basal ganglia and rostral thalami, as well as the left pulvinar”. There was no sign of more widespread of diffuse signal changes as you might see with ADEM (acute disseminated encephalomyelitis) or cerebellar changes as you might see with enterovirus. No hemorrhagic changes, as with herpes simplex. The laterality and location of the damage matched the physical symptoms (motor dysfunction affecting the right more than left), but more importantly it was also similar to previous reported scans from patients with arthropod-borne flaviviruses, including Powassan. Choi and Taylor wrote in a 2012 case report “MRI images of the patient’s central nervous system (CNS) were unique, and when such images are encountered in the clinical setting, Powassan viral infection should be considered.” We were able to test the baby’s spinal fluid at the CDC for Powassan, and it came back positive.
The points to make about this case are several – firstly, the recurring comment from most (probably all) of my colleagues when I made the diagnosis was “What made you think of it?” Honestly, it was mostly the fact that I had training in a state where Powassan was well-known and we would consider it routinely. I simply added it to the differential and saw that not only could I not rule it out, I had some evidence to support it! But the issue here is that there were probably many cases of Powassan over the years that doctors had been seeing, but simply never thought of testing. Powassan was not on a routine viral encephalitis panel in Connecticut (it’s a send-out to the CDC), whereas some other State laboratories like New York test for it automatically on their own encephalitis panel, in addition to sending/reporting to the CDC. It is very much a case of out of sight, out of mind.
Secondly, even if some physicians had considered and tested for the virus somehow, Connecticut didn’t make Powassan a reportable disease until 2019 (more than 2 years after I made the first diagnosis in the state). It’s really hard to measure something if you’re not counting it…and of course even hard to count something if you’re not looking for it!
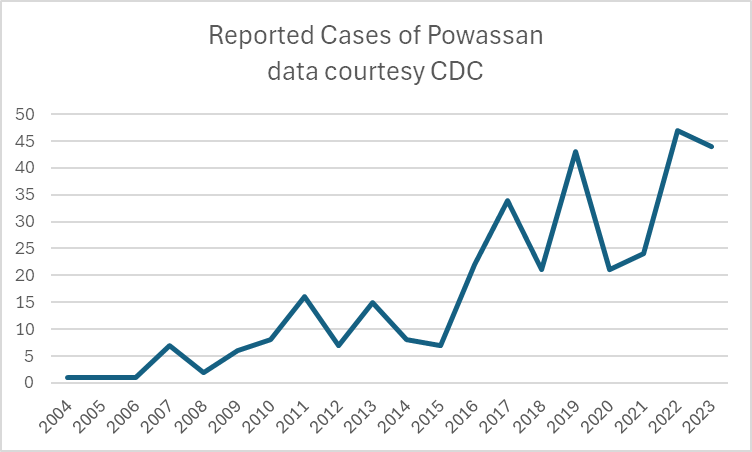
So this makes it really, really hard to know what to do with news that “Powassan cases are increasing.” Reports are increasing, but so is awareness, and testing availability – it doesn’t mean that actual infections with the virus are going up. It is possible that they are…but the case reports alone aren’t enough to make that conclusion. You really have to understand the reporting infrastructure and testing limitations in the context of a specific disease when trying to interpret the changes you might see in any sort of incidence or prevalence data.
There isn’t a vaccine yet for Powassan virus, although when I last checked research was ongoing (and there is a vaccine for TBE). The best way to prevent infection is to avoid any kind of tick exposure at all – cover skin, use DEET, avoid tramping through the wilderness in areas where the virus is known to be in ticks, and check your pets! Also – change your clothing when you get indoors from activities that might have exposed you to ticks…
Bonus if you’ve made it this far – you can check out my TV appearance on Monsters Inside Me below!